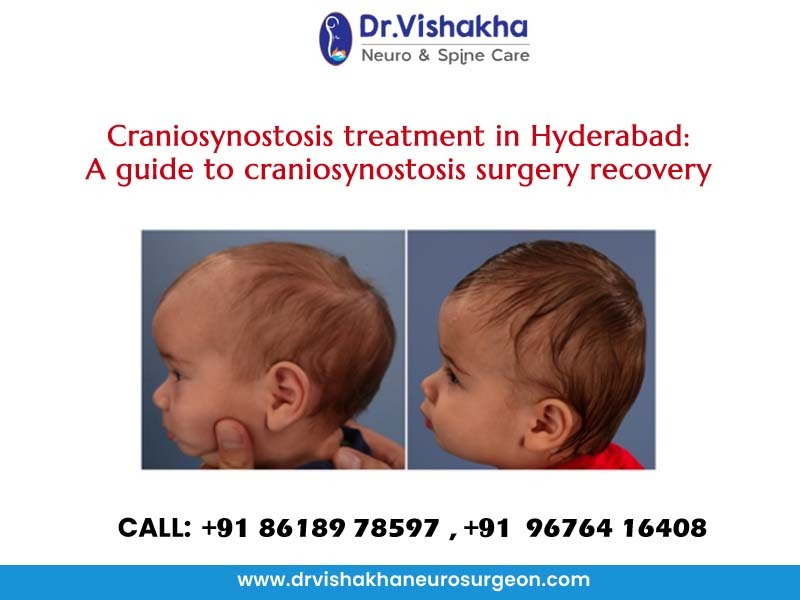
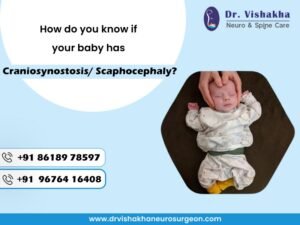
Craniosynostosis is a congenital condition in which one or more of the sutures in an infant’s skull close prematurely. These sutures are fibrous joints that connect the skull bones and allow for growth of the brain during early development. When a suture fuses too early, it can restrict skull growth in certain areas, leading to an abnormal head shape and potentially causing increased pressure on the brain.Symptoms may include an irregular head shape, developmental delays, and, in some cases, increased intracranial pressure. Treatment usually involves surgery to correct the skull shape and allow for normal brain growth, often performed in the first year of life. Early diagnosis and intervention are essential for optimal outcomes.
Craniosynostosis treatment in Hyderabad by Dr.Vishakha

Treatment for craniosynostosis typically involves surgery to correct the abnormal head shape and ensure proper brain development. The primary goals of the treatment are to allow for normal growth of the skull and to alleviate any intracranial pressure that may have developed. Here are the key aspects of craniosynostosis treatment:
- Surgical Intervention: Surgery is often recommended within the first year of life, as this is when the skull is still malleable, making it easier to reshape.The specific surgical technique may vary depending on the type and severity of craniosynostosis, but it generally involves making an incision, removing the fused suture, and reshaping the skull bones.
Surgeons may use techniques such as:
– Open Cranial Vault Remodeling: This involves a larger incision and removal of portions of the skull to reshape it.
– Endoscopic Suturectomy: A less invasive approach in which small incisions are made to remove the fused suture, often used in certain cases and followed by helmet therapy.
- Helmet Therapy: In some cases, after surgery, infants may be fitted with a special cranial helmet to help guide the growth of the skull into a more normal shape. This can help prevent further deformities as the child grows.
- Monitoring and Follow-Up Care: Continuous monitoring of the child’s development is essential after surgery. Follow-up appointments with a pediatrician and a specialist (such as a pediatric neurosurgeon or craniofacial surgeon) will help ensure that the child is developing normally and that there are no complications.
- Physical Therapy: If there are associated developmental delays or positional issues (such as torticollis), physical therapy may be recommended to help improve muscle strength and coordination.
- Parental Support and Education: Providing education and support to parents about what to expect during recovery and the overall developmental journey of their child is an important aspect of treatment.
Surgical intervention typically results in improved head shape and allows for normal brain growth, leading to better long-term outcomes. Early diagnosis and treatment are key to minimizing potential complications associated with craniosynostosis.
Dr.Vishakha’s guide to craniosynostosis surgery recovery

Recovery from craniosynostosis surgery typically involves several stages, and while individual experiences may vary, here’s a detailed overview of what to expect during the recovery process:
Immediately After Surgery
- Recovery Room Monitoring: Post-surgery, the child will be moved to a recovery room where medical staff will closely monitor vital signs, consciousness levels, and pain management as the anesthesia wears off.
- Pain Management: Children may feel discomfort after the operation, and pain relief will be provided through medication. It’s essential to assess pain levels regularly to ensure the child is comfortable.
Hospital Stay
- Length of Stay: The hospital stay after craniosynostosis surgery can vary, usually lasting from one to three days, depending on the child’s condition and recovery progress.
- Monitoring for Complications: During the hospital stay, healthcare providers will monitor for any potential complications, such as bleeding, infection, or excessive swelling.
- Intravenous (IV) Fluids: Initially, the child may receive IV fluids to ensure proper hydration and nutrition until they can tolerate oral intake.
Initial Recovery Phase (1-2 weeks)
- Rest and Activity Limitations: After returning home, it’s crucial for the child to rest. Physical activity, including running or jumping, should be significantly limited for a specified period (usually several weeks) to allow healing.
- Incision Care: Parents will need to monitor the surgical site for signs of infection, such as increased redness, swelling, or discharge. Keeping the area clean and dry is vital, and the surgeon will provide specific instructions for care.
- Follow-Up Appointments: Follow-up visits with the surgeon are typically scheduled within a week or two after surgery to assess healing and determine whether any additional treatment is necessary.
Intermediate Recovery Phase (2-6 weeks)
- Swelling and Bruising: Swelling around the forehead and eyes is common and may take several weeks to subside. Cold compresses may help alleviate discomfort and reduce swelling.
- Diet: A soft diet may be recommended initially, depending on the child’s comfort level. Gradual reintroduction of solid foods can occur as the child recovers.
- Gradual Return to Activities: After the initial recovery period, parents can slowly reintroduce normal activities, though contact sports and high-risk activities should remain avoided for a longer duration.
Long-Term Recovery (6 weeks and beyond)
- Cranial Helmet: If prescribed, a cranial helmet may be used for several months post-surgery to help shape the skull as it continues to grow. Regular visits with a specialist will ensure proper fitting and monitoring.
- Developmental Monitoring: Regular follow-up appointments will also focus on the child’s development, as some may require additional support such as physical therapy for coordination or muscle strength.
- Parental Support and Education: Parents should be aware of the signs of complications and the importance of attending all follow-up appointments. Support groups or resources may be beneficial as families navigate the recovery process.
Emotional and Psychological Considerations
- Child’s Adjustment: Children may need time to adjust to the physical changes following surgery. They may also experience emotional responses related to the procedure. Support from parents and caregivers is critical during this adjustment phase.
- Encouragement and Reassurance: Providing emotional support and reassurance as the child adapts to their new appearance and experiences can be integral to their overall recovery process.
Overall, most children recover well from craniosynostosis surgery, with many experiencing significant improvements in skull shape and a favorable outcome in terms of cognitive and developmental milestones. The recovery process is critical and closely monitored to ensure a healthy transition back to normalcy.
About Dr Vishakha:
Dr Vishakha Basavraj Karpe is a highly skilled senior consultant at Rainbow Children’s Hospital in Banjara Hills and Hydernagar Hyderabad. She is known for her comprehensive care approach and is one of the few dedicated leading paediatric neurosurgeons in the city and India with over ten years of extensive experience in pediatric neurosurgery. Her expertise includes treating hydrocephalus, spinal dysraphism, craniosynostosis, paediatric brain infections, brain and spine tumours and stroke surgery. She has a special interest in craniosynostosis surgery, which is done only in very few centres in India.
Proficiency of Dr Vishakha:
-
- Hydrocephalus (increased fluid in the brain): The procedure involves an endoscopic third ventriculostomy and CSF diversion (VP shunt) to treat complex hydrocephalus.
- Craniosynostosis (abnormal head shape due to untimely cranial sutures fusion) surgeries: Helmet therapy is a technique that is used in both endoscopic and open surgery.
- Spinal dysraphisms(Spina Bifida)- (spinal abnormalities present by birth) – surgical repair
- Encepahaocles repair surgery.
-
- Vascular conditions and stroke surgeries: revascularization surgeries for moya moya disease.
- Pediatric brain and spine tumour surgeries.
-
- Pediatric brain and spine infection surgeries: Endoscopic and open surgeries for brain and spine infections.
- Pediatric traumatic brain and spinal injury.
- Antenatal counselling for congenital fatal neurosurgical conditions.