Dr. Vishakha Karpe
MBBS, DNB(Surg) , MCH (neurosurgery), MRCS (UK),
Fellowship in neuroendoscopic surgery.
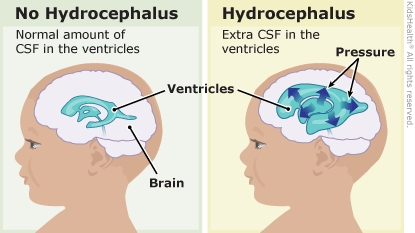
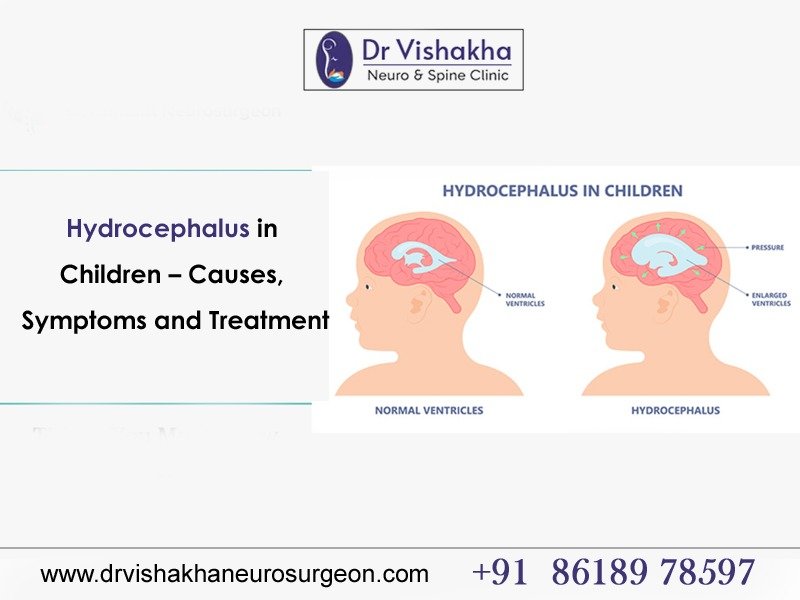
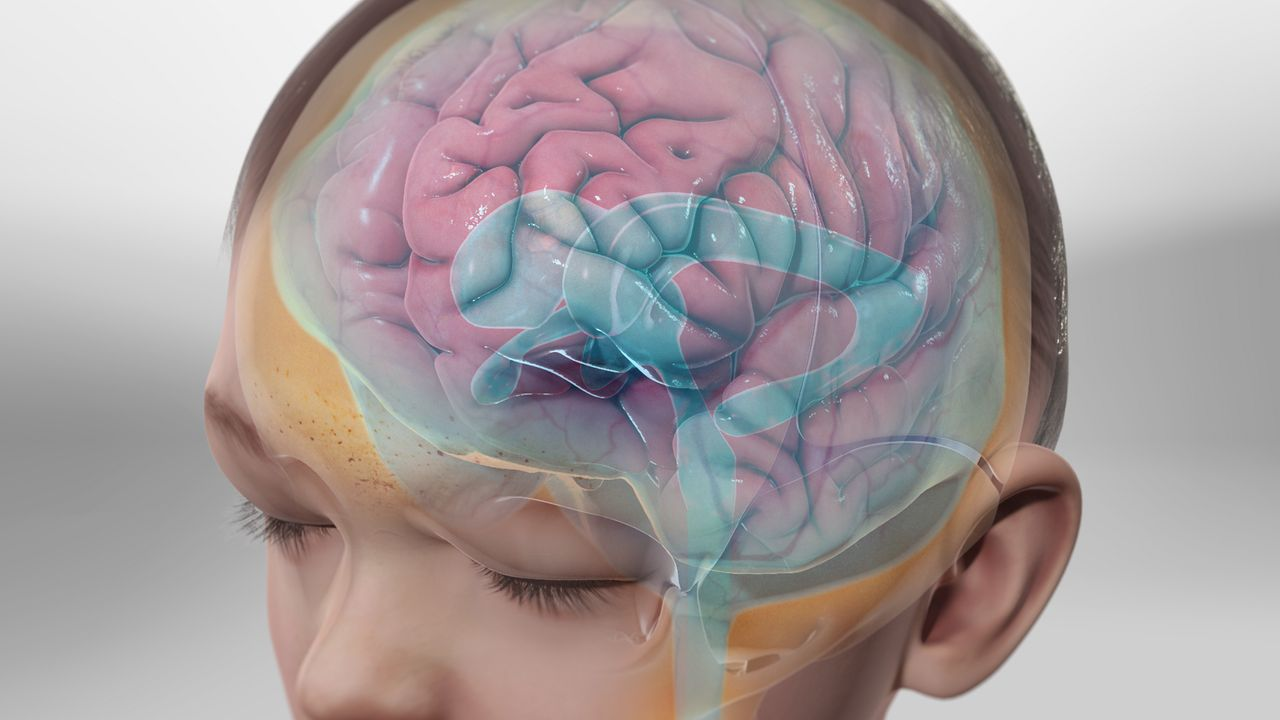
Hydrocephalus is a condition in children where cerebrospinal fluid (CSF) accumulates abnormally within the brain’s ventricles, causing increased pressure on the brain. It can be due to blockages in CSF flow or overproduction, causing ventricles to enlarge and potentially causing damage. Hydrocephalus can occur at birth or develop later in infancy or childhood. Common causes include congenital abnormalities, infections, brain bleeding, intraventricular haemorrhage, tumours, or traumatic brain injury rarely O neural tube defects. Hydrocephalus in children can cause symptoms like an enlarged head, vomiting, irritability, sleepiness, poor feeding, seizures, and developmental delays. Treatment often involves a surgical intervention create a new pathway for CSF drainage inside the brain, or implant a shunt system to divert excess fluid away from the brain. Early diagnosis and treatment are crucial to prevent complications and minimise the impact on a child’s development and quality of life.
Causes of hydrocephalus in children:
- Congenital abnormalities:
Birth-induced structural abnormalities can disrupt the normal cerebrospinal fluid (CSF) flow, resulting in hydrocephalus.
- Aqueductal stenosis:
The aqueduct of Sylvius, is a communication between 3rd and 4th ventricles which helps CSF move between ventricles. Blockage of this level can cause problems in fluid circulation leading to excessive accumulation.

- Neural tube defects:
Hydrocephalus, also known as spina bifida or encephalocele, occurs when the neural tube fails to seal completely during fetal development.
- Dandy-walker syndrome:
Congenital cerebellar and fourth ventricle malformations are frequently associated with hydrocephalus.
- Infections:
Infections affecting the brain and its surrounding structures can cause inflammation, scarring, and obstruction of CSF flow, leading to hydrocephalus.
- Meningitis:
The inflammation of the brain and spinal cord membranes can result in the blockage of CSF pathways.
- Ventriculitis
The infection of ventricles can disrupt the circulation of CSF.
- Bleeding:
Premature infants or those with traumatic injuries may experience brain bleeding, leading to blood accumulation that blocks CSF pathways.
- Intraventricular haemorrhage (IVH):
Premature infants often experience bleeding into the ventricles of the brain due to fragile blood vessels.
- Tumors:
Brain tumors, both benign and malignant, can impede CSF flow, causing hydrocephalus, either within the brain or from nearby structures.
- Ependymoma:
Tumors are formed by the spinal cord’s ventricles and central canal cells.
- Medulloblastoma:
A malignant tumor typically found in the cerebellum can obstruct CSF pathways.
- Traumatic brain injury:
Head trauma, including falls, motor vehicle accidents, or shaken baby syndrome, can cause brain damage, bleeding, swelling further leading to hydrocephalus.
- Other causes:
- Arachnoid cysts:
Fluid-filled sacs form between the brain or spinal cord in the arachnoid membrane.
- Intracranial hemorrhage:
Vascular malformations or coagulation disorders can cause severe bleeding.
Early diagnosis and treatment are crucial for managing hydrocephalus, often involving surgical interventions to restore average CSF circulation and alleviate brain pressure.
Symptoms of hydrocephalus in children:
Hydrocephalus symptoms in children vary based on age, cause, and fluid accumulation rate.
- Changes in the head of infants due to hydrocephalus:
- The infant has a head that is larger than usual.
- The infant’s head size rapidly increases.
- A tense, bulged or tense soft spot on the top of the head.
- Physical symptoms:
- Nausea and vomiting.
- Sleepiness or sluggishness, known as lethargy.
- Irritability.
- Poor eating.
- Seizures.
- Downward deviation of the eyes (sunsetting sign).
- Problems with muscle tone and strength.
II. Symptoms of hydrocephalus among younger and older children:
- Headache.
- Blurred or double vision.
- Eye movements that are not usual.
- Enlargement of a toddler’s head.
- Trouble with balance.
- Delayed developmental milestones
- Poor coordination.
- Poor appetite.
- Loss of bladder control or urinating often.
Diagnosis of hydrocephalus in children:
- Clinical assessment:
- Medical history:
The healthcare provider will gather information about the child’s symptoms, developmental milestones, birth history, medical conditions, and family history of hydrocephalus or related disorders.
- Physical examination:
A comprehensive neurological examination will evaluate the child’s neurological function, including reflexes, muscle strength, coordination, and signs of increased intracranial pressure like tense soft spot, and enlarged head circumference.
-
- Ophthalmological evaluation (Eye examination) : It is important to look for effects of raised pressure in brain on the eye nerves and to rule out visual impairment.
- Imaging studies:
- Ultrasound:
Cranial ultrasound is frequently used in infants to detect hydrocephalus, providing crucial insights into ventricle size and structural abnormalities.
- CT scan (computed tomography):
CT imaging aids in visualizing brain structures, assessing ventricle size and configuration, and identifying underlying causes of hydrocephalus, such as tumors or hemorrhages.
- MRI (magnetic resonance imaging):
MRI offers detailed brain images, confirms hydrocephalus diagnosis, evaluates brain damage, and identifies abnormalities, aiding in surgical planning.
- Monitoring hydrocephalus in children:
- Head circumference measurement:
Serial head circumference measurements are crucial in infants to detect abnormal growth patterns that may indicate hydrocephalus.
- Intracranial pressure monitoring:
In cases of uncertainty about hydrocephalus diagnosis or surgical intervention, invasive monitoring of intracranial pressure can be used to assess its severity and guide treatment decisions.
- CSF analysis:
If hydrocephalus is suspected to be caused by infection or bleeding, cerebrospinal fluid analysis via lumbar puncture may be necessary to detect inflammation, infection, or blood.
Early hydrocephalus diagnosis is crucial for optimal treatment, requiring a multidisciplinary approach involving pediatricians, neurologists, neurosurgeons, radiologists, and other healthcare professionals for comprehensive evaluation and management.
Treatment for hydrocephalus in children:
Hydrocephalus treatment often involves surgical intervention to alleviate brain pressure caused by CSF accumulation.
- Shunt surgery: Ventriculoperitoneal (VP) shunt
The most common treatment involves a shunt system, a flexible tube placed in the brain’s ventricles to drain excess CSF from the brain to the abdominal cavity, with a valve to regulate CSF flow and prevent over-drainage or under-drainage.
Programmable shunts are the advanced type of shunts where the valve pressure can be changed externally even after surgery.
- Endoscopic third ventriculostomy (ETV):
An endoscopic procedure involves creating a new opening in the third ventricle floor for cerebral aqueduct blockage, allowing CSF to divert to the area where it will be absorbed
- Treatment for underlying causes:
If hydrocephalus is a secondary condition to another condition like a tumor or infection, it may be necessary to treat the underlying cause in addition to hydrocephalus treatment.
- Regular monitoring:
Regular healthcare professional monitoring is crucial for children with hydrocephalus to effectively manage the condition, ensure proper functioning of the shunt, and address potential complications.
Early diagnosis and treatment are crucial for preventing complications and minimizing the impact on a child’s development and quality of life.
Prognosis for hydrocephalus in children:
Hydrocephalus prognosis in children varies significantly based on factors like the cause, severity, diagnosis age, treatment timeline, and individual response to interventions.
- Early detection and treatment:
Early diagnosis and management of hydrocephalus in children, often through surgical intervention like shunt or ETV, can improve prognosis, prevent further brain damage, and optimize long-term outcomes.
- Effectiveness of treatment:
Treatment effectiveness, including CSF drainage and control of pressure in the brain, significantly influences prognosis. Regular monitoring and adjustments may be necessary to manage complications or changes over time.
- Underlying cause:
The prognosis of hydrocephalus, particularly in cases involving neural tube defects, tumors, or infections, can be influenced by the management and outcomes of the underlying condition.
- Developmental outcomes:
Hydrocephalus affects children’s cognitive, motor, and behavioral development, causing delays in learning, memory, attention, motor skills, and social-emotional functioning. However, support services, educational interventions, and rehabilitation can lead to meaningful progress.
- Complications:
Hydrocephalus complications, including shunt malfunction, infection, seizures, and developmental disabilities, can significantly impact a child’s prognosis and quality of life, necessitating prompt recognition and management.
- Long-term monitoring:
Hydrocephalus children require ongoing healthcare monitoring for neurodevelopmental progress, complications, and treatment adjustments, with regular follow-up appointments crucial for optimal outcomes and timely resolution of emerging issues.
Hydrocephalus is a chronic condition that requires ongoing management, but many children can lead fulfilling lives with appropriate medical care, support services, and interventions, requiring close collaboration with healthcare providers.
About Dr Vishakha :
Dr Vishakha Basavraj Karpe, a highly skilled senior consultant at Rainbow Children’s Hospital in Banjara Hills and Hydernagar Hyderabad. She is known for her comprehensive care approach and is one of the few dedicated leading paediatric neurosurgeons in the city and India with over ten years of extensive experience in pediatric neurosurgery. Her expertise includes treating hydrocephalus, spinal dysraphism, craniosynostosis, paediatric brain infections, and brain and spine tumours and stroke surgery.
She has special interest in craniosynostosis surgery, which is done only in very few centres in India.
Proficiency of Dr Vishakha:
-
- Hydrocephalus (increased fluid in the brain): The procedure involves an endoscopic third ventriculostomy and CSF diversion (VP shunt) to treat complex hydrocephalus.
- Craniosynostosis (abnormal head shape due to untimely cranial sutures fusion) surgeries: Helmet therapy is a technique that is used in both endoscopic and open surgery.
- Spinal dysraphisms(Spina Bifida)- (spinal abnormalities present by birth) – surgical repair
- Encepahaocles repair surgery.
-
- Vascular conditions and stroke surgeries: revascularization surgeries for moya moya disease.
- Pediatric brain and spine tumour surgeries.
-
- Pediatric brain and spine infection surgeries: Endoscopic and open surgeries for brain and spine infections.
- Pediatric traumatic brain and spinal injury.
- Antenatal counselling for congenital fatal neurosurgical conditions.