A brachial plexus injury (BPI) in children occurs when the network of nerves controlling movement and sensation in the shoulder, arm, and hand is damaged. These nerves originate from the spinal cord and branch out to the upper limbs. BPI can occur at any age and results from nerves connecting the neck to the arms, hands, and fingers being stretched, squeezed, or cut. The nerves extend from the neck to the fingers.
Types of brachial plexus injuries symptoms and causes
An avulsion is a severe brachial plexus injury where a nerve is completely disconnected from the spinal cord, preventing regeneration and causing permanent loss of function. It often leads to arm paralysis, sensation loss, and Horner’s syndrome, affecting the face and eye.
Causes of brachial plexus injuries
Obstetric avulsion can occur due to various birth-related causes, including difficult labour, shoulder dystocia, breech birth, and the use of forceps or vacuum extraction. These factors can cause excessive force on the baby’s head and neck, nerve stretching, and increased stress on the brachial plexus, ultimately increasing the risk of avulsion.
Traumatic avulsion can occur due to various non-birth-related causes, including motor vehicle accidents, falls or sports injuries, heavy trauma or blunt force injuries, and nerve tumours or infections. These injuries can cause sudden nerve damage, causing avulsion in the shoulder or neck.

Symptoms of brachial plexus injuries
Nerve damage can cause symptoms such as complete arm paralysis, loss of sensation, severe pain, muscle atrophy, and weak reflexes. If these symptoms persist or worsen, seek medical attention. Horner’s syndrome, a condition characterized by drooping eyelids, small pupils, and reduced sweating, can be caused by the avulsion of C8-T1 nerves. Severe cases may lead to spinal cord damage. If these symptoms persist or worsen, it is imperative to seek medical attention.
Diagnosis
Early diagnosis of avulsion injuries is crucial for treatment planning. Doctors check for muscle weakness, reflex loss, and sensation loss in the arm, as well as Horner’s syndrome. Imaging tests like MRI, CT Myelography, EMG and NCS are used to identify nerve root avulsions, scar tissue, and nerve activity, confirming nerve root detachment from the spinal cord.
Recovery and Prognosis
Avulsion injuries require early treatment, surgical success, and rehabilitation for long-term recovery. Mild cases can recover partially within 1-2 years, while severe cases require multiple surgeries and may not return to full function. Without treatment, permanent arm paralysis and muscle atrophy occur. With surgery, partial movement recovery is possible, but strength may be reduced. Rehabilitation is crucial for maximum improvement.
Treatment
Surgical treatment
Nerve transfer is the best treatment for avulsion injuries, replacing damaged nerves with healthy ones. Muscle or tendon transfer restores movement if nerve repair isn’t possible. Free Functional Muscle Transfer (FFMT) transfers a thigh muscle to the arm, including its nerve and blood supply. Common nerve transfers in avulsion cases include spinal accessory nerve to suprascapular nerve, intercostal nerves to musculocutaneous nerve, and phrenic nerve to brachial plexus.
Non-surgical treatment
Non-surgical treatments for children without surgery include physical therapy, occupational therapy, splints and braces, and pain management through medications or nerve blocks. These therapies help maintain joint mobility, prevent stiffness, and adapt to daily activities, ensuring proper function and safety.
What is a rupture injury?
A rupture is a severe brachial plexus injury where a nerve is completely torn but not detached from the spinal cord, requiring surgical intervention to restore function. The severity of functional loss depends on the number of ruptured nerves and the location of the rupture, resulting in muscle weakness or paralysis.
Causes
A rupture occurs when the brachial plexus nerves are subjected to extreme stretching, pulling, or trauma, causing them to tear. Birth-related causes like difficult labour and shoulder dystocia increase stress on the brachial plexus. Non-birth causes like motor vehicle accidents, falls, sports injuries, blunt force trauma, and surgical complications also contribute. Surgical complications are rare, and medical procedures rarely damage the brachial plexus.
Symptoms
A rupture in the ribs can cause common symptoms such as weakness or paralysis in the affected arm, loss of muscle control, loss of sensation, abnormal arm posture, muscle atrophy due to nerve signal loss, and reduced reflexes. Associated symptoms include Erb’s Palsy (C5-C6 Rupture), Klumpke’s Palsy (C8-T1 Rupture), and Total Brachial Plexus Injury (C5-T1 Rupture), which can result in complete paralysis of the entire arm. The severity of the rupture depends on the affected nerves and the number of torn nerves.
Diagnosis
Early diagnosis of nerve rupture is crucial for determining surgery needs. Physical examinations include muscle strength and movement testing, sensory testing, and reflex testing. Imaging tests like MRI and CT Myelography help visualize nerve tears and scar tissue formation. EMG and NCS measure electrical activity in muscles to determine nerve damage severity. Inconclusive results may require CT Myelography for nerve rupture detection.
Recovery and prognosis
Recovery from a rupture depends on early treatment and the effectiveness of surgery and therapy. Mild ruptures may take 6-12 months, while severe ruptures may take over two years. Without surgery, permanent function loss occurs. Early surgery and therapy can lead to significant improvement in movement and strength, while without treatment, permanent weakness or paralysis may occur. Lifelong therapy may be necessary for maximum recovery.
Treatment
Surgical treatment
Nerve grafting is a surgical procedure where a damaged nerve is replaced with a healthy donor from another part of the body. Nerve transfer is used when direct repair is not feasible, transferring a healthy nerve to replace the damaged nerve’s function. Muscle or tendon transfer is used when nerve repair is insufficient to restore movement. Common nerve transfers for rupture injuries include spinal accessory nerve suprascapular nerve, intercostal nerves, musculocutaneous nerve, and median or ulnar nerve radiolar nerve.
Non-surgical treatment
Rehabilitation is essential for regaining function after surgery, involving physical therapy, occupational therapy, splints and braces, and pain management through medications or nerve blocks for neuropathic pain, preventing stiffness, strengthening muscles, and assisting with daily tasks.
What is neuroma?
A neuroma is a brachial plexus injury where a nerve is partially torn or stretched, causing scar tissue to form around the damaged nerve. This scar tissue disrupts normal nerve signals, causing pain, weakness, or loss of function. While they don’t completely cut off nerve function, they can significantly interfere with movement and sensatiby labourometimeslabouriring surgical treatment.
Causes
Neuromas in brachial plexus injuries can be caused by trauma, nerve injury, surgical scarring, compression or chronic irritation, or delayed or improper healing. Trauma occurs when a stretched or partially torn nerve tries to heal, leading to scar tissue formation. Improper healing or inflammation can also result in neuroma formation.
Symptoms
Neuromas cause a variety of symptoms, including persistent pain, burning or tingling sensations, touch sensitivity, muscle weakness, limited range of motion, and abnormal nerve sensations. If untreated, severe symptoms may include chronic pain, severe muscle weakness or paralysis, and permanent nerve damage, leading to loss of sensation. Common symptoms include persistent pain, burning sensations, sensitivity to touch, muscle weakness, and limited range of motion.
Types of neuromas
- End-neuroma is a condition resulting from an injury, causing pain, sensitivity, and a burning sensation at the severed end of a nerve.
- Contusion Neuroma is a condition characterized by mild pain, weakness, and partial loss of function due to the bruising of a nerve.
- Adherent neuroma occurs when a nerve heals incorrectly and attaches to surrounding tissues, causing pain, stiffness, and reduced movement.
- Stump Neuroma is a condition resulting from nerve amputation or unsuccessful nerve repair, causing severe pain, abnormal sensations, and muscle weakness.
Diagnosis
A neuroma is diagnosed through physical exams and imaging tests to assess nerve function and scar tissue formation. Physical examinations include palpation tests, range of motion testing, nerve sensitivity tests, and imaging tests like MRI and ultrasound. MRI detects scar tissue around nerves, ultrasound identifies nerve thickening and abnormal tissue, and electromyography and nerve conduction studies measure the efficiency of nerve signal transmission.
Treatment
Surgical Interventions for Severe or Persistent Neuroma Cases
Neuroma surgery is necessary for chronic pain or major functional loss caused by a neuroma. The surgery involves neuroma excision, nerve grafting, nerve transfer, and targeted muscle reinnervation (TMR). Excision removes scarred nerve tissue, nerve grafting replaces damaged sections with healthy ones, nerve transfer connects a nearby working nerve to the affected nerve, and TMR redirects nerve endings to muscles for severe neuromas with amputations.
Non-surgical
Neuromas can be treated conservatively through physical therapy, pain medications, nerve blocks, desensitization therapy, and splints or braces. These treatments help reduce pain, improve movement, and reduce sensitivity to touch. They also include anti-inflammatory drugs, nerve pain medications, nerve blocks, desensitization therapy, and preventing excessive movement that may worsen pain.
Recovery and prognosis
Neuroma recovery depends on the severity of the injury and treatment. Mild cases, treated with therapy, can improve within weeks to months, while surgical cases take 6 to 12 months. Severe cases involving multiple neuromas and nerve grafts may take 1-2 years for full function improvement. Early treatment leads to significant pain relief and functional improvement, while without treatment, chronic pain and nerve damage may occur.
What is Neurapraxia?
Neurapraxia is a mild nerve injury where the nerve remains intact but temporarily stops functioning due to compression, stretching, or trauma. The injury disrupts nerve signal transmission, causing temporary weakness or loss of function. Unlike severe nerve injuries, Neurapraxia is fully reversible and usually recovers without surgery.
Causes
Neurapraxia is a condition causing temporary nerve disruption due to external pressure, trauma, or overstretching. Birth-related causes include obstetric Neurapraxia, caused by prolonged labor or shoulder dystocia, while non-birth-related causes include blunt trauma, compression injuries, hyperextension, and mild electrical injuries. Obstetric Neurapraxia is caused by prolonged pressure on the baby’s shoulder and neck.
Symptoms
Neurapraxia is a temporary and reversible condition characterized by weakness or temporary paralysis in the affected limb, numbness or tingling, loss of sensation but no muscle atrophy, burning, electric shock-like pain in severe cases, and reflex loss or sluggish reflexes. Common symptoms include Erb’s Palsy (C5-C6 Neurapraxia), Klumpke’s Palsy (C8-T1 Neurapraxia), and “Stinger” or “Burner” Syndrome (Common in Athletes), which results in sudden burning pain, numbness, or weakness in the arm after an impact to the neck or shoulder.
Diagnosis
Neurapraxia is diagnosed clinically, involving physical examination, muscle strength testing, sensation testing, and reflex testing. Imaging and nerve tests, such as MRI, ultrasound, and EMG, are used to confirm the extent of the injury. These tests check for weakness, movement limitations, numbness, tingling, and diminished reflexes and confirm normal nerve continuity without rupture or avulsion. These tests help diagnose and treat nerve issues.
Prognosis
Surgical treatment
Neurapraxia doesn’t require surgery unless severe compressions, like a tumour or scar tissue, are present. Nerve decompression surgery is needed for prolonged pressure, like cysts or bone spurs, and exploratory nerve surgery is needed in rare cases where symptoms persist beyond recovery time.
Non-surgical treatment
Neurapraxia treatment focuses on symptom relief, preventing stiffness, and speeding up recovery. First-line treatments include rest and activity modification, physical therapy and rehabilitation, pain management with NSAIDs or nerve pain medications, splints or braces to reduce nerve stress, and desensitization therapy to manage tingling or hypersensitivity as nerves recover. These non-surgical treatments aim to prevent stiffness and improve overall recovery.
Brachial neuritis is a condition that can change over time, causing pain, weakness, tingling, or numbness. It often follows a shoulder or nerve injury and requires prompt treatment. An accurate diagnosis is crucial as it may mimic symptoms of other diseases. A doctor can suggest various treatment methods to alleviate pain and discomfort. The recovery period is long and requires a strong commitment to rehabilitation. Maintaining a positive outlook and seeking support from friends, family, and healthcare providers is essential. Management focuses on preventing deficits and maximizing a child’s capabilities. Supportive and encouraging behaviour, positive reinforcement, and a healthy sense of self-esteem promote independence.
About Dr Vishakha:
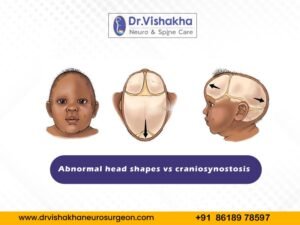
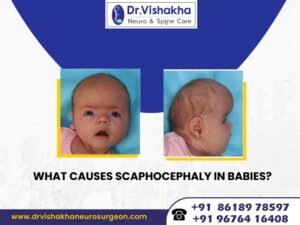
Dr Vishakha is a highly skilled senior consultant at Rainbow Children’s Hospital in Banjara Hills and Hydernagar Hyderabad. She is known for her comprehensive care approach and is one of the few dedicated leading paediatric neurosurgeons in the city and India with over ten years of extensive experience in pediatric neurosurgery. Her expertise includes treating hydrocephalus, spinal dysraphism, craniosynostosis, paediatric brain infections, brain and spine tumours and stroke surgery. She has a special interest in craniosynostosis surgery, which is done only in very few centres in India.
Proficiency of Dr Vishakha:
-
- Hydrocephalus (increased fluid in the brain): The procedure involves an endoscopic third ventriculostomy and CSF diversion (VP shunt) to treat complex hydrocephalus.
- Craniosynostosis (abnormal head shape due to untimely cranial sutures fusion) surgeries: Helmet therapy is a technique that is used in both endoscopic and open surgery.
- Spinal dysraphisms(Spina Bifida)- (spinal abnormalities present by birth) – surgical repair
- Encepahaocles repair surgery.
-
- Vascular conditions and stroke surgeries: revascularization surgeries for moya moya disease.
- Pediatric brain and spine tumour surgeries.
-
- Pediatric brain and spine infection surgeries: Endoscopic and open surgeries for brain and spine infections.
- Pediatric traumatic brain and spinal injury.
- Antenatal counselling for congenital fatal neurosurgical conditions.